Ovary cancer incidence and mortality in China, 2011
Introduction
Ovary cancer is one of the female common cancers. According to GLOBOCAN 2012, there were 238,719 new and 151,905 death ovary cancer cases in the world in 2012, ovary cancer was the top 7 female incident and death cancer worldwide in 2012, its incident age-standardized rate by world standard population (ASR-W) and death ASR-W were 6.1/100,000 and 3.7/100,000, respectively. In China, there were 34,575 new and 14,676 death ovary cancer cases in 2012. It was the top 10 female incident and top 13 female death cancer in China in 2012, and its incident and death ASR-Ws were 4.1/100,000 and 1.7/100,000, respectively (1). There were increasing trends for its incidence and mortality in 2003-2007 in 32 Chinese selected cancer registering areas, and its incident age-standardized rate by Chinese standard population (ASR-C) and death ASR-C increased from 4.53/100,000 and 1.58/100,000 in 2003 to 5.15/100,000 and 1.77/100,000 in 2007, respectively, increased by 13.70% and 12.31%, respectively (2). According to the estimation by the National Central Cancer Registry of China (NCCR), ovary cancer was the top 9 female incident cancer and top 3 incident female genital cancer in China, and its incident ASR-C was 5.22/100,000, only slightly lower than that of corpus uteri cancer (5.84/100,000) in 2010 (3). Hence, ovary cancer was a major female health concern. For providing scientific information for its control and prevention, this paper analyzed the ovary cancer incident and death status in China in 2011 based on the cancer data from 177 Chinese cancer registries.
Material and methods
Incidence and mortality data
Ovary cancer incident and death data came from NCCR. NCCR is responsible for cancer data collection, evaluation and publication from local population-based cancer registries. The cancer information was reported to the cancer registries from local hospitals and community health centers, including the Basic Medical Insurances for Urban Residents and the New-Rural Cooperative Medical System. The Vital Statistical Database was linked with the cancer incidence database for identifying cases with death certificate only (DCO) and follow-up. All cancer cases were classified according to the International Classification of Diseases for Oncology, 3rd edition (ICD-O-3) and the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) (3). Invasive cases of ovary cancer (ICD10: C56) were extracted and analyzed from the overall 2011 cancer database. The incidence and mortality data were based on the data from the 177 population-based cancer registries, which distributed in 28 provinces (77 in urban and 100 in rural areas) and covered 175,310,169 population accounting for about 13.01% of the whole Chinese population, including 88,655,668 males and 86,654,501 females, 98,341,507 in urban and 76,968,662 in rural areas, and the data quality met the quality criteria [as follows: the percentage of cases morphologically verified (MV%) was between 66-85%, the percentage of death certificate-only cases (DCO%) and the percentage of unknown basis (UB%) were lower than 10%, and the mortality/incidence (M/I) ratio was between 0.6-0.8] required by NCCR.
Population data
The population was estimated based on the fifth National Population Census data [2000] provided by the National Statistics Bureau of China, taking into account of the changes of age composition, gender ratio and the proportion of urban and rural transformation released by the National Bureau of Statistics (http://data.stats.gov.cn/). The national population in 2011 was stratified by area (urban/rural) and age groups (0-, 1-4, 5-84 by 5 years, 85+ years). The changes of age-specific death probability were also adjusted when calculating population. Linear changes were assumed in each age group between the fifth and sixth Population Census.
Statistical analysis
Incident and death cases, proportions, crude, standardized, accumulated, truncated and age-specific incidences and mortalities were calculated by area and age groups. The numbers of new cases and deaths were estimated using the 5-year age-specific cancer incidence/mortality rates and the corresponding populations. The Chinese population in 2000 and World Segi’s population were used for age-standardized rates. The cumulative risk of developing or dying from ovary cancer before 75 years of age (in the absence of competing causes of death) was calculated and presented as a percentage. Software including MS-Excel and IARCcrgTools2.05 issued by International Agency for Research on Cancer (IARC) and International Association of Cancer Registries (IACR) (4) was used for data checking and evaluation. SAS software (SAS Institute Inc., Cary, USA) was used to calculate the incidence and mortality rates.
Results
Data quality
Total 177 registries, 77 in urban and 100 in rural areas, accepted by NCCR for publishing the annual cancer registry report, from which ovary cancer data were extracted, distributed in 28 provinces, and covered 175,310,169 populations accounting for 13.01% of total Chinese population in 2011, including 88,655,668 males and 86,654,501 females, 98,341,507 in urban and 76,968,662 in rural areas.
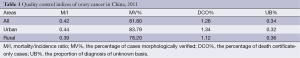
The ovary cancer quality indicators of MV%, DCO% and M/I ratio overall in this study were 81.80%, 1.26% and 0.42, respectively, 83.79%, 1.34% and 0.44 for urban registries, respectively, and 78.20%, 1.12% and 0.39 for rural registries, respectively, with urban indicators higher than rural. The quality evaluation for ovary cancer in this study is presented in Table 1.
Full table
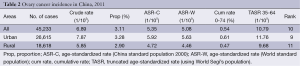
Incidence
It was estimated there were 45,223 new ovary cancer cases, accounting for 3.11% of all new female cancer cases in China in 2011. The crude, ASR-C and ASR-W incidence were 6.89/100,000, 5.35/100,000 and 5.08/100,000, respectively. Ovary cancer was the top 10 incident cancer in all female cancers. Among the patients aged 0-74 years old, the cumulative incidence rate was 0.54%. The crude and age-standardized incident rates in urban areas were higher than those in rural areas (Table 2).
Full table
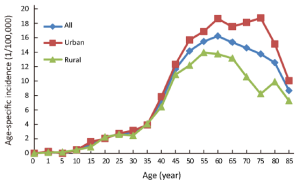
Age-specific incidence
The age-specific incidence rate of ovary cancer in China in 2011 was at low level before age 35-39, although it began to increase from age 10-14 and dramatically from age 35-39 years. It peaked at age 60-64 years and declined significantly thereafter. But in urban areas, it remained stable after peaking at age 60-64 and decreased quickly from age 75-79, while in rural areas, it declined slowly after peaking at age 55-59 and declined quickly from age 65-69. Before age 45-49, the age-specific incidence rates in urban and rural areas were close to each other, thereafter the rates in urban areas were much higher than those in rural areas, but next to each other again at age 85+ (Figure 1).
Mortality
It was estimated there were 18,430 cases died from ovary cancer, accounting for 2.40% of all female cancer deaths in 2011 in China. The crude, ASR-C and ASR-W mortality were 2.81/100,000, 2.01/100,000 and 1.99/100,000, respectively. Ovary cancer was the top 12 death cancer in all female cancers. Among the patients aged 0-74 years, the cumulative mortality was 0.23%. The death crude rate and ASRs in urban areas were higher than those in rural areas (Table 3).
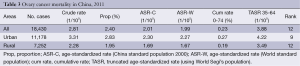
Full table
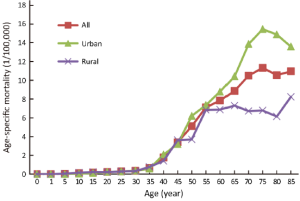
Age-specific mortality
The age-specific mortality of ovary cancer was at very low level until it increased dramatically from age 35-39 years in China in 2011. It peaked at age 75-79 and remained stable thereafter. But in urban areas, it declined obviously after peaking, and in rural areas, it remained relatively stable after age 55-59 and peaked at age 85+ years. Before age 55-59, the age-specific mortality rates in urban areas were next to the rates in rural areas, but significantly higher than those in rural areas thereafter (Figure 2).
Discussion
In order to ensure the quality of registration data, NCCR only received the data which met the data quality criteria of NCCR for including in the Chinese cancer registries annual report (3). Through the double evaluations in provincial and national level, 177 registries were qualified and accepted for final database. The valid data were pooled and analyzed for cancer statistics in 2011. Although the data quality indicators such as MV%, DCO% and M/I ratio in this paper were basically close to the indicators in 2012 Chinese cancer registries annual report (5), Chinese cancer incidence and mortality 2003-2007 (2) and annual report on status of cancer in China, 2010 (3), the indicators in this study, especially the M/I ratio, were at lower level compared with the indicators in the registries, especially the ones from North America and Europe, included in the Cancer Incidence in Five Continents version X (6). It suggested that the ovary cancer data quality in this study should be improved.
GLOBOCAN 2012 estimated that ovary cancer incident and death ASRs in 2012 in the world were 6.1/100,000 and 3.7/100,000, respectively, 9.1/100,000 and 5.0/100,000 in the developed areas, respectively, 5.0/100,000 and 3.1/100,000 in the underdeveloped areas, respectively, 5.0/100,000 and 3.0/100,000 in Asia, respectively, 4.1/100,000 and 1.7/100,000 in China, respectively (1). Compared with GLOBOCAN 2012 data, the ovary cancer incidence in this study was lower than that of world, obviously lower than that of developed areas, close to the rates of Asia and underdeveloped areas. The mortality in this study was lower than that of world, Asia and underdeveloped area, significantly lower than that of developed areas. Both incidence and mortality in this study were slightly higher than the Chinese rates estimated by GLOBOCAN 2012 (1).
GLOBOCAN 2012 also divided the world into several areas according to ovary cancer incidence and mortality: high incident (ASR >8.4/105) and death (ASR >5.5/105) areas, middle-high incident (6.8-8.4/105) and death (4.4-5.5/105) areas, middle incident (5.0-6.8/105) and death (3.5-4.4/105) areas, middle-low incident (3.8-5.0/105) and death (2.8-3.5/105) areas, and low incident (<3.8/105) and death (<2.8/105) areas. High incident areas were major in Europe and developed areas, but Fiji in South America and Arabia in Middle East were also with high incidence, and high death areas were in Melanesia, Central and Eastern Europe and Northern Europe. Low incidence areas were in Micronesia and Western Africa, and low death areas were in Eastern Asia and Micronesia. Compared with GLOBOCAN 2012 data, China was in the middle ovary cancer incident areas and low death areas in 2011 (1).
The top 5 countries with ovary cancer incidence in the world in 2012 were Fiji (ASR-W 14.9/105), Latvia (14.2/105), Bulgaria (14.0/105), Poland (13.6/105) and Serbia (12.8/105), while the top 5 countries in Asia were Singapore (9.9/105), Kazakhstan (9.7/105), Brunei (8.8/105), Armenia (8.5/105) and Indonesia (8.4/105). The top 5 countries with ovary cancer mortality in the world in 2012 were Fiji (9.8/105), Latvia (8.8/105), Lithuania (8.4/105), Poland (7.3/105) and Ireland (6.9/105), while the top 5 in Asia were Indonesia (6.1/105), Kazakhstan (6.0/105), Brunei (6.0/105), Armenia (5.1/105) and Israel (5.1/105). China was not in the top 20 countries with ovary cancer incidence and mortality (1). Its incidence in this study was close to the rates of Lao (5.2/105), Bhutan (5.2/105), Timor-Leste (5.1/105) and India (4.9/105), and its mortality was close to the rates of Vietnam (1.9/105), Tajikistan (1.8/105), Azerbaijan (1.7/105) and Uzbekistan (1.7/105) in 2012 according to GLOBOCAN 2012 (1). Ovary cancer incident and death rates in this paper were close to the incident and death rates in Chinese cancer incidence and mortality 2003-2007 (2), annual report on status of cancer in China, 2010 (3) and 2012 Chinese cancer registries annual report (5).
Generally, ovary cancer incidence and mortality in developed and urban areas were higher than those in less developed and rural areas. The incidence and mortality in developed areas in 2012 were 1.82 and 1.61 times higher than that in underdeveloped areas, respectively (1). The incident and death ASR-Ws in the Chinese urban registering areas in 2009 were 1.65 and 1.84 times higher than that in the Chinese rural registering areas, respectively (5), and in 2003-2007, 2.74 and 2.15 times higher than that in the Chinese rural registering areas, respectively (2). The incident ASR-C in the Chinese urban registering areas was 1.39 times higher than that in the Chinese rural registering areas in 2010 (3). But the top 3 areas with ovary cancer incidence in 2009 Chinese registering areas were Yunmeng County of Hubei province (11.08/105), Sihui City of Guangdong province (10.32/105) and Qingyang District of Chengdu City of Sichuan province (9.88/105), two of which (Yunmeng County and Sihui City) were in rural areas. The top 3 areas with ovary cancer mortality were Lianyungang City Center of Jiangsu province (5.61/105), Guangzhou City (3.10/105) and Sihui City of Guangdong province (3.33/105), one of which (Sihui City) was in rural areas. The incidence and mortality in Nangan district of Haerbing City in Heilongjiang Province, Huaiying and Chuzhou districts of Huaian City in Jiangsu province, which were urban areas, Shexian County in Hebei province, and Donggan and Taixian City in Jiangsu province, which were rural areas, were at low levels (5).
Ovary caner etiology is complicated, and its incident mechanism is not clear totally. Many factors such as biology, psychology, environment, female hormone, pregnancy, lactation, menstruation, viral infection, diet, genetics, cancer gene and mind were related with its incidence. Worse environment, increasing pace of life, more mind pressure, irrational diet and less exercise may be associated with its increasing incidence (2,7). Its mortality was also related with the diagnosis, treatment, economic and education levels. Difference in the incidence and mortality of ovary cancer among different areas may be caused by the above factors.
Ovary cancer incidence and mortality were at high levels among the incidence and mortality of female genital system cancers, especially, its mortality was 2 times in the world and Asia and 2 times more higher in the developed and underdeveloped areas than that of corpus uteri cancer, close to it in China in 2012 (1). It indicated ovary cancer control should be enhanced.
Some difference existed between the age-specific incidence and mortality in this paper and those of Chinese registering areas in 2003-2007 (2) and 2009 (5). The age-specific incidence and mortality in this paper peaked at age 60-64 years and declined quickly, but remained stable after age 50-54 and down rapidly after peaking at age 65-69 in 2003-2007 (2) and 2009 Chinese registering areas (5). The age-specific incidence in urban areas in this paper was close to the rates of rural areas before age 45-49 years and after age 85+, but in 2003-2007 (2) and 2009 (5) Chinese registering areas, they were close to each other before age 40-44 years. The age-specific mortality in urban areas in this paper was close to that of rural areas before age 55-59 years, but they were close to each other before age 40-45 in 2003-2007 and 2009 Chinese registering areas (2,5).
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Ferlay J, Soerjomataram I, Ervik M, et al. GLOBOCAN 2012 v1.0, cancer incidence and mortality worldwide: IARC CancerBase No. 11. Lyon: IARC, 2013. Available online: http://globocan.iarc.fr, accessed on October 18, 2014.
- National Cancer Centre, Bureau for Disease Control and Prevention of Health Ministry. Chinese cancer incidence and mortality, 2003-2007. Beijing: Military Medical Science Press, 2012;17:251-8.
- Chen W, Zheng R, Zhang S, et al. Annual report on status of cancer in China, 2010. Chin J Cancer Res 2014;26:48-58. [PubMed]
- Ferlay J. The IARC crgTools Programs. Lyon: IARC, 2006. Available online: http://www.iacr.com.fr
- National Cancer Center, Disease Prevention and Control Bureau, MOH. Chinese Cancer Registry Annual Report (2012). Beijing: Military Medical Science Press, 2012;17:87-92,118-52.
- Forman D, Bray F, Brewster DH, et al. Cancer Incidence in Five Continents, Vol. X (electronic version). Lyon: IARC, 2013. Available online: http://ci5.iarc.fr, accessed on October 18, 2014.
- Boyle P, Levin B. World Cancer report 2008. Lyon: IARC, 2008:424-7.