Application of CUSA Excel ultrasonic aspiration system in resection of skull base meningiomas
Introduction
Intracranial meningiomas are common brain tumors derived from arachnoidal cells and account for about 30% of primary brain tumors (1-3). Most meningiomas are histologically classified as benign tumors (WHO grade I), however, about 10% represent atypical (WHO grade II) or anaplastic (WHO grade III) subtypes (2-5). Generally, the optimal therapy of meningioma is surgical removal. However, for those tumors located on skull base and sphenoid ridge still remain a big challenge due to its complex anatomic relationships among tumor, blood vessels and cranial nerves, especially when the tumors are hard and tough (6). Here, we applied the CUSA Excel ultrasonic aspiration system in skull base meningioma resection, which was introduced into our department three months ago. The advantage of the new technique is to protect the vessels and nerves during tumor resection.
Patients and methods
Patient information
A total of 10 patients with anterior, middle skull base and sphenoid ridge meningioma were operated using the CUSA Excel ultrasonic aspiration system at the Department of Neurosurgery in Shanghai Huashan Hospital from August 2014 to October 2014. There were six male and four female patients, aged from 38 to 61 years old (the mean age was 48.5 years old). A total of five cases with tumor located at anterior skull base, three cases with tumor on middle skull base, and two cases with tumor on sphenoid ridge. The tumor situation is listed in Table 1.
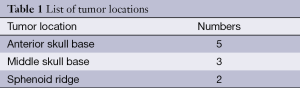
Full table
CT & MRI examination
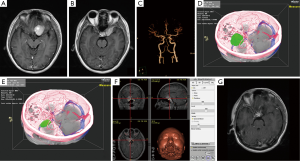
Preoperative CT and MRI scanning with contrast enhancement were performed in all patients. Brain magnetic resonance angiography (MRA) was also performed by Siemens 3T MRI scanner. The three dimensional time-of-flight MRA (3D-TOF MRA) sequence was used and the scanning parameters were as follows: TR =21 ms, TE =3.6 ms, FOV =200 mm, averages =1, slice thickness =0.9 mm. The images data were post-processed by maximum intensity projection (MIP) in the workstation to display the relationships of the tumor and its supplying arteries (6).
Virtual reality (VR) planning
All the patients’ imaging data of brain CT, MRI and MRA were transferred to a VR workstation (Dextroscope, Volume Interactions, Singapore) (6). The images were processed within the RadioDexter software (Volume Interactions) in order to display the 3D stereoscopic images of tumor and its adjacent supplying arteries, including internal carotid artery (ICA) and its branches such as anterior cerebral artery (ACA) and middle cerebral artery (MCA), which makes the relationship of tumor and vessels more real and vivid.
Neuronavigation
A Medtronic navigational system (Treon, Medtronic Stealthstation) was used in all surgical manipulations (7). The day before surgery, at least 6-8 fiducials were placed on the patients in a scattered pattern for reference prior to imaging and for viewing on the resulting images. Brain CT, MRI and MRA data of the patients were input into the workstation of the navigation system. Registration was performed in the operating room by touching the markers with the probe while indicating to the surgical workstation where marker was being touched. After registration, the lesion on the scalp projection was localized for surgical incision.
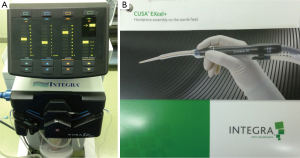
Operation and CUSA Excel
During the operation, we applied the CUSA Excel ultrasonic aspiration system (Figure 1). It’s a new machine produced by Integra Lifesciences corporation and has been introduced into our department for just three months. The most valuable advantage of this technique is its tissue selection during operation, thus it could avoid brain vessels and nerves injury.
Results
Here, we chose one case for illustration of the CUSA Excel ultrasonic aspiration system. It’s a 46-year-old male patient, suffered from headache and vision decrease. Pre-operation brain MRI showed meningioma located on the left middle skull base and sphenoid ridge (Figure 2). The patient was performed craniotomy and tumor resection after consent. During the operation, the CUSA Excel ultrasonic aspiration system was used to help resect the tumor (Figure 3). Due to the close relationships of the tumor and its surrounding vessels and nerves, we carefully operated on the tumor. Our experience is that the optimal parameters for vessel and nerve preservation are as follows: the suction is 60 Hz, the hitting power is 80 Hz, and the paramount of tissue select (Figure 4). For more operating procedures reference, please go to the company websites.


Discussion
Meningiomas arise from meningeal arachnoidal cells, and they account for about 30% of all primary brain tumors (1-3). The optimal therapy of intracranial meningiomas is surgical removal. Most benign meningiomas (WHO grade I) have good prognosis after surgical resection, while malignant meningiomas (WHO grade II and III) that may relapse postoperatively (9). However, resection of anterior and middle skull base meningiomas is still difficult due to the complex anatomy structures and the close relationships of tumor and its adjacent arteries and nerves, especially when the tumors are very hard and tough.
The CUSA Excel ultrasonic aspiration system is a helpful tool during the operation (10,11). We have just introduced a new CUSA Excel in our department, which was produced by Integra Lifesciences Corporation. It could help resect the tumor while protect the vessels and nerves surrounding the tumor during operation if the neurosurgeons choose the optimal operating parameters. This new system was easy to set up and use. The hand piece was not heavy and didn’t disturb the view of the neurosurgeon even in keyhole surgical fields (just like the case in our report). We didn’t experience any injuries to vessels or nerves during tumor resections.
Conclusions
In conclusion, our experiences in the ten cases of skull base meningiomas resection indicated that the CUSA Excel ultrasonic aspiration system is really a sensitive tool, and could help to avoid the damage to important brain vessels and nerves during brain tumor resection.
Acknowledgements
We are grateful to Professor Ying Mao, deputy director of Department of Neurosurgery in Huashan Hospital, for his advice on paper writing.
Funding: The study was supported by National Natural Science Foundation of China (81200936, 81372707), and Shanghai Committee of Science and Technology (12JC1401800).
Disclosure: The authors declare no conflict of interest.
References
- Wang DJ, Xie Q, Gong Y, et al. Histopathological classification and location of consecutively operated meningiomas at a single institution in China from 2001 to 2010. Chin Med J (Engl) 2013;126:488-93. [PubMed]
- Riemenschneider MJ, Perry A, Reifenberger G. Histological classification and molecular genetics of meningiomas. Lancet Neurol 2006;5:1045-54. [PubMed]
- Mawrin C, Perry A. Pathological classification and molecular genetics of meningiomas. J Neurooncol 2010;99:379-91. [PubMed]
- Tang H, Sun H, Xie L, et al. Intraoperative ultrasound assistance in resection of intracranial meningiomas. Chin J Cancer Res 2013;25:339-45. [PubMed]
- Perry A, Louis DN, Scheithauer BW, et al. Meningiomas. In: Louis DN, Ohgaki H, Wiestler OD, et al. eds. WHO Classification of Tumours of the Central Nervous System. Lyon: IARC, 2007:163-72.
- Tang HL, Sun HP, Gong Y, et al. Preoperative surgical planning for intracranial meningioma resection by virtual reality. Chin Med J (Engl) 2012;125:2057-61. [PubMed]
- Mao Y, Zhou L, Du G, et al. Image-guided resection of cerebral cavernous malformations. Chin Med J (Engl) 2003;116:1480-3. [PubMed]
- Tang H, Zhang H, Xie Q, et al. Intraoperative application of the CUSA Excel ultrasonic aspiration system. Asvide 2014;1:357. Available online: http://www.asvide.com/articles/391
- Alexiou GA, Gogou P, Markoula S, et al. Management of meningiomas. Clin Neurol Neurosurg 2010;112:177-82. [PubMed]
- Jallo GI. CUSA EXcel ultrasonic aspiration system. Neurosurgery 2001;48:695-7. [PubMed]
- Schroeteler J, Reeker R, Suero Molina E, et al. Glioma tissue obtained by modern ultrasonic aspiration with a simple sterile suction trap for primary cell culture and pathological evaluation. Eur Surg Res 2014;53:37-42. [PubMed]